References
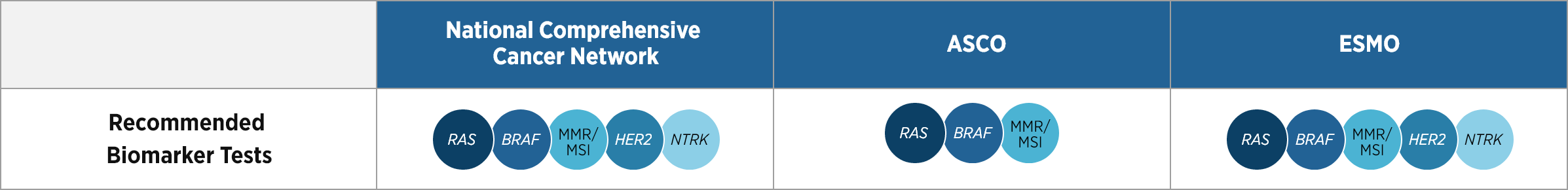
1. Morris VK, Kennedy EB, Baxter NN, et al. J Clin Oncol. 2023;41:678-700.
2.
Doleschal B, Petzer A, Rumpold H. Front Oncol. 2022;12:1048166. 3. Cohen R, Pudlarz T, Delattre JF,
Colle R, André T. Cancers (Basel). 2020;12:2350. 4. Peeters M, Kafatos G, Taylor A, et al.
Eur J Cancer. 2015;51:1704-1713. 5. Pietrantonio F, Di Nicolantonio F, Schrock AB, et al.
Ann Oncol. 2018;29:1394-1401. 6. Referenced with permission from the NCCN Clinical
Practice Guidelines in Oncology (NCCN Guidelines®) for Colon Cancer V.5.2025. © National Comprehensive
Cancer Network, Inc.
2025. All rights reserved. Accessed November 24, 2025. To view the most recent and complete version of the
guideline, go online to NCCN.org. NCCN makes no warranties of any kind whatsoever regarding their content,
use or application and disclaims any responsibility for their application or use in any way.
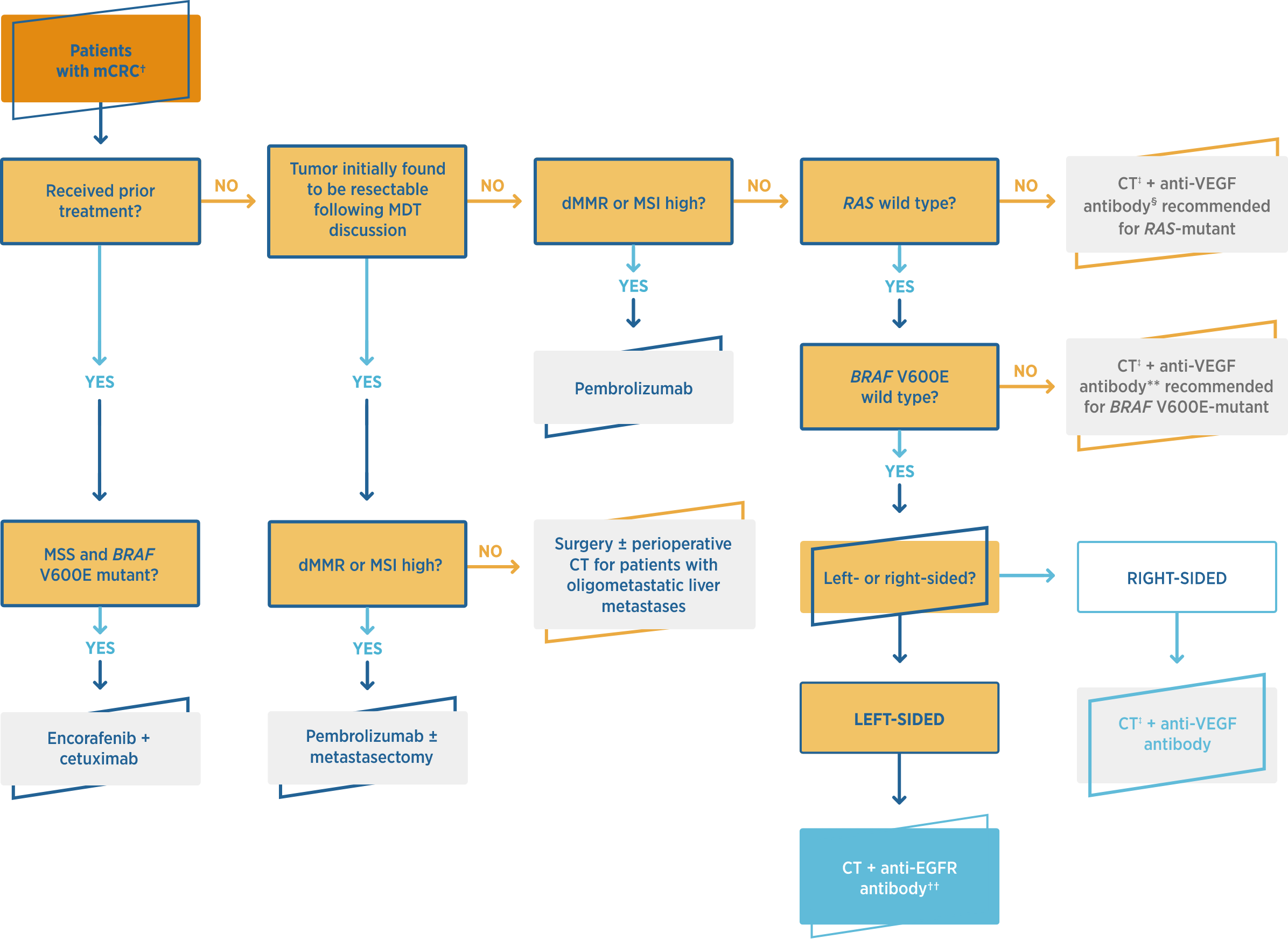
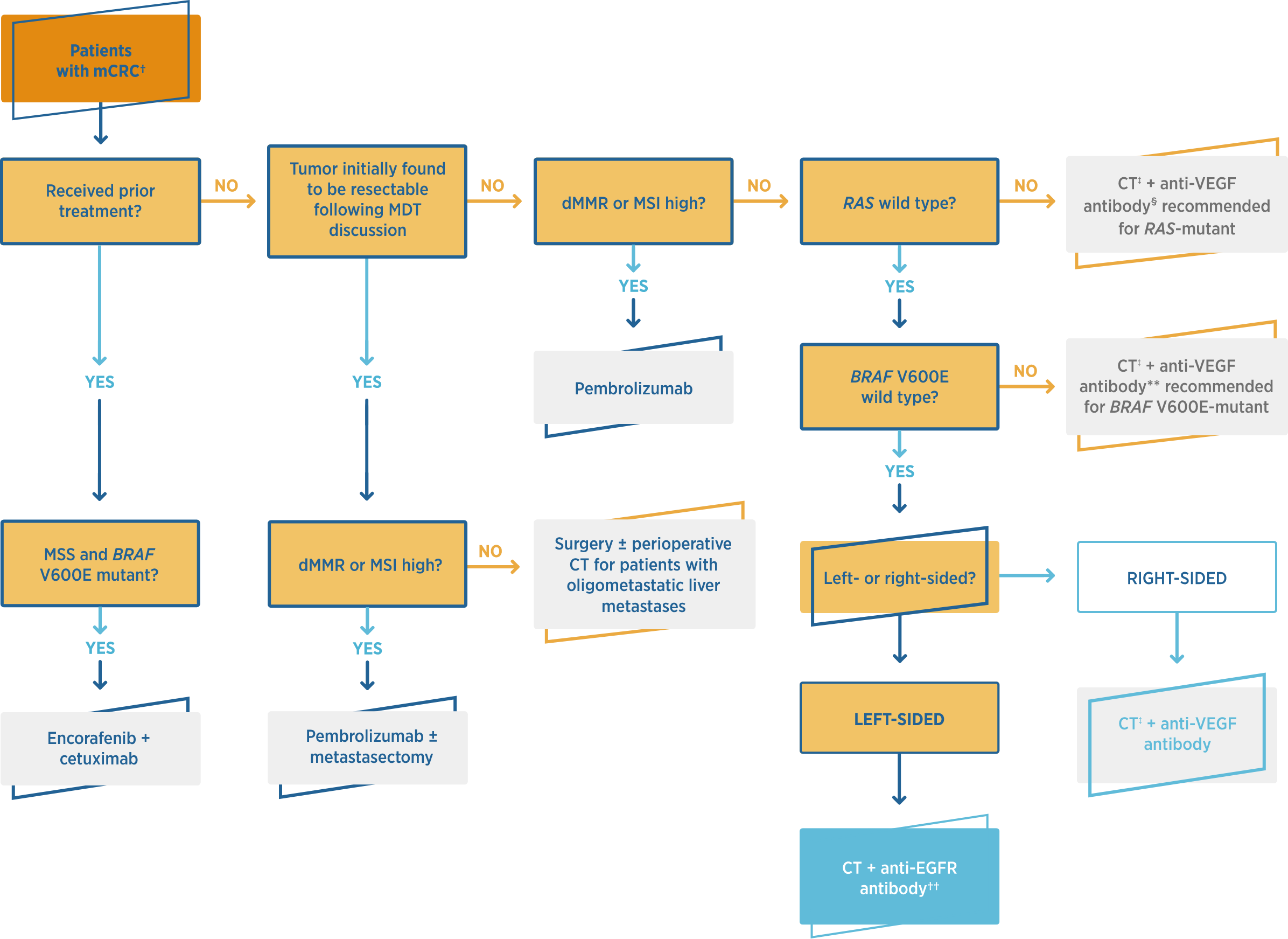
7. Systemic therapy for metastatic colorectal cancer (mCRC) algorithm. ASCO
Guidelines®. 2022. 8. Nevala-Plagemann C, Iyengar S, Trunk AD, Pappas L, Haaland
B, Garrido-Laguna I. J Natl Compr Canc Netw. 2022;20(3):268-275. 9. Iyer P, Deng M,
Handorf
EA, Nakhoda S, Dotan E. JNCI Cancer Spectr. 2022;6:pkac065. 10. Robinson HR, et al. Poster
presented at: American Society of Clinical Oncology (ASCO) Gastrointestinal Cancers Symposium; January
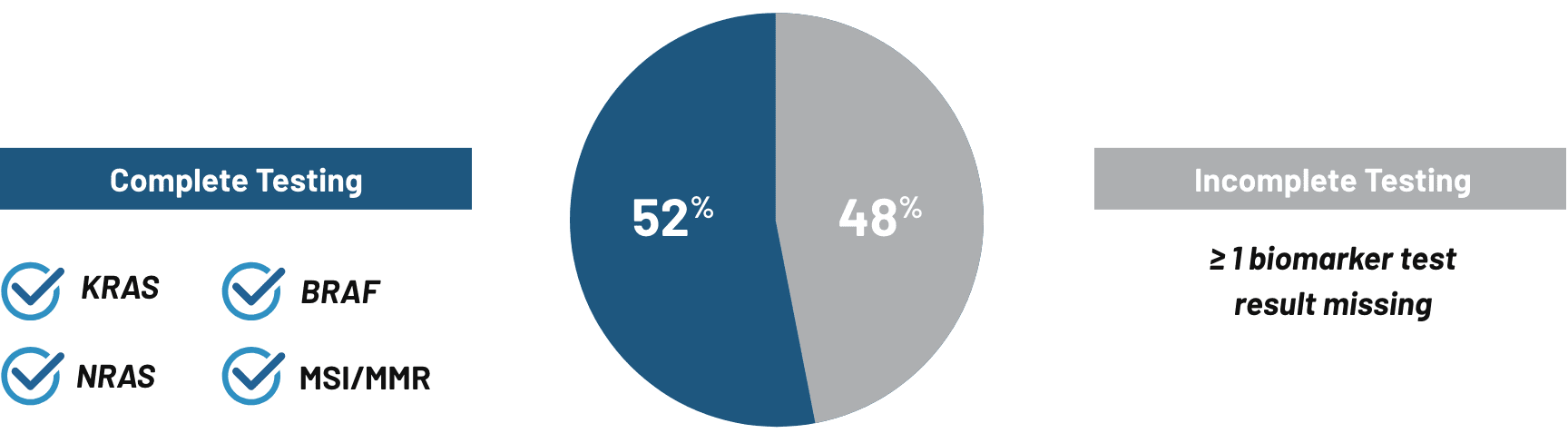
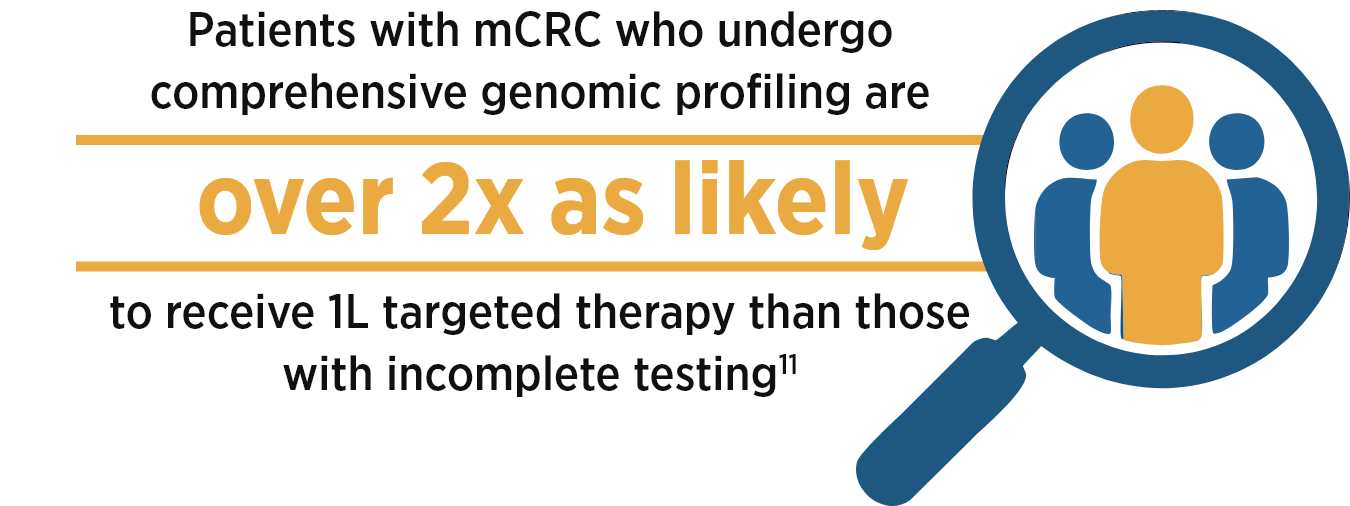
18-20, 2024; San Francisco, CA. 11. Byfield S, Bapat B, Becker L, et al. JAMA Netw Open.
2025;8(7):e2519963. doi:10.1001/jamanetworkopen.2025.19963. 12. Byfield S, Bapat B, Becker
L, et al. JAMA Netw Open. 2025;8(7)(suppl):e2519963. doi:10.1001/jamanetworkopen.2025.19963.
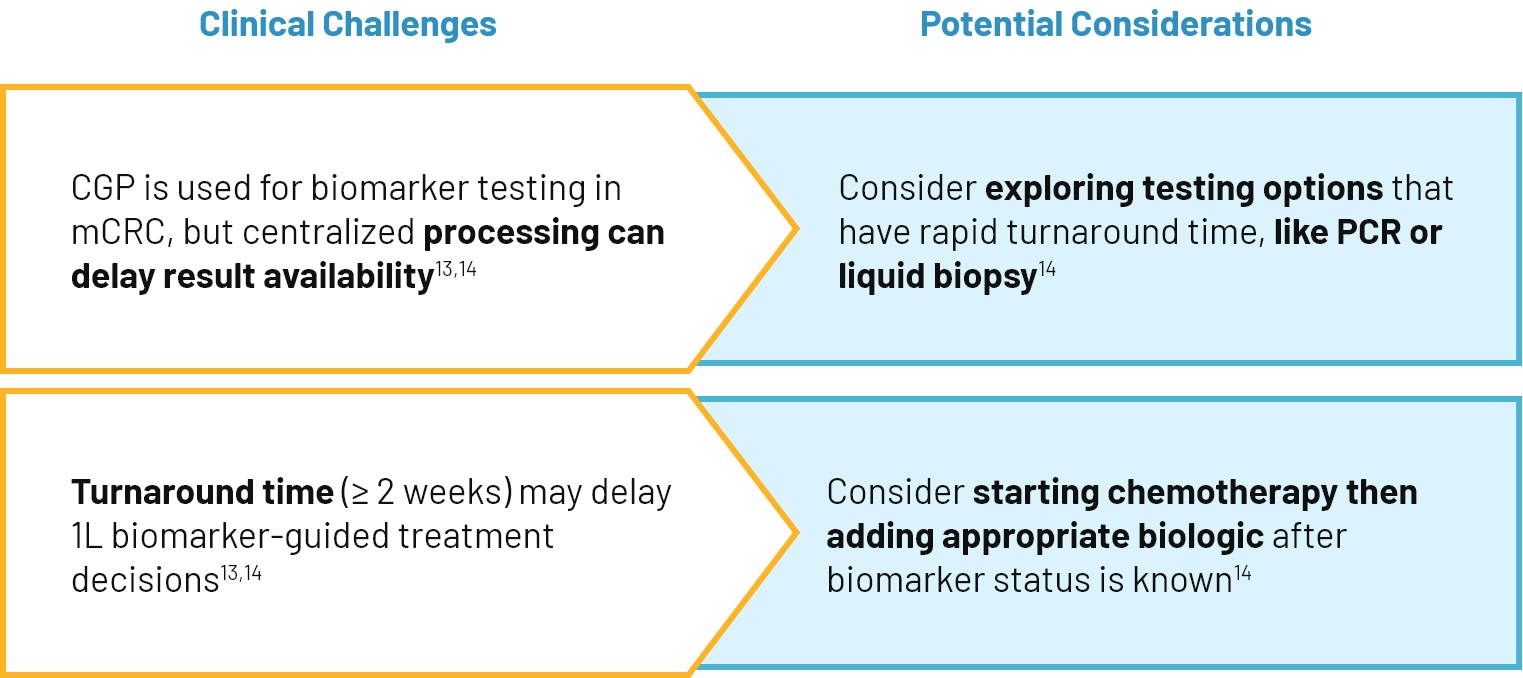
13. Fiala O, Veskrnova V, Chloupkova R, et al. Target Oncol. 2018;13(6):735-743.
14. Palmieri LJ, Antoun S, Falandry C, et al. The Oncologist. 2019;24(6):e353-e360.
15. Sepulveda AR, Hamilton SR, Allegra CJ, et al. J Clin Oncol. 2017;35:1453-1486.
16. Cervantes A, Adam R, Roselló S, et al. Ann Oncol. 2023;34:10-32. 17.
El-Deiry WS, Goldberg RM, Lenz HJ, et al. CA Cancer J Clin. 2019;69:305-343. 18. Pennell
NA, Arcila ME, Gandara DR, West H. Am Soc Clin Oncol Educ Book. 2019;39:531-542.
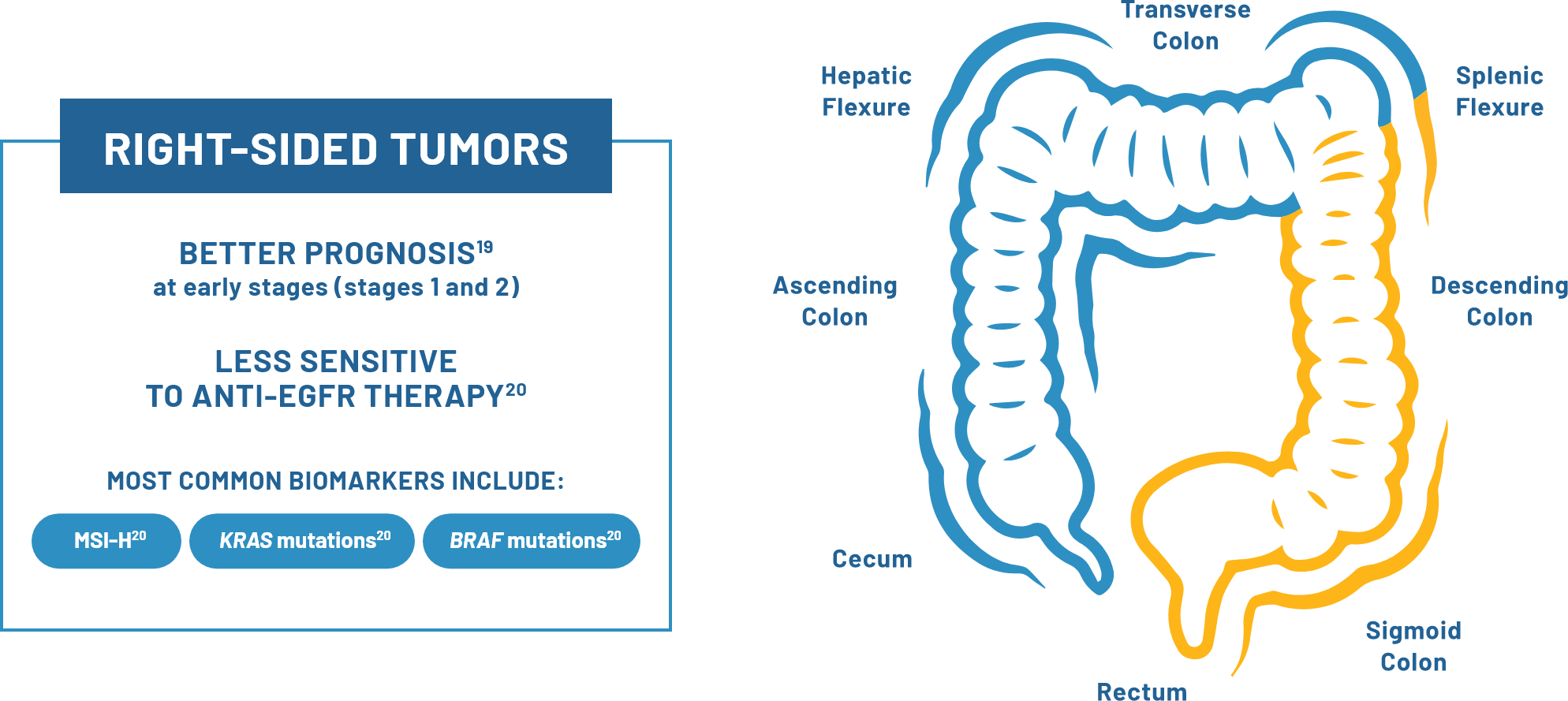
19. Baran
B, Mert O, Acar E, et al. Gastroenterol Res. 2018;11(2):123-132. 20. Waldstein S, Spengler
M, Pinchuk IV, Yee NS. J Pers Med. 2023;13(7):1114. 21. Vectibix® (panitumumab)
prescribing
information, Amgen.