INDICATION AND LIMITATION OF USE
Vectibix® is indicated for the treatment of patients with wild-type RAS (defined as wild-type in both KRAS and NRAS as determined by an FDA-approved test for this use) metastatic colorectal cancer (mCRC):Read More
Vectibix® is indicated for the treatment of patients with wild-type RAS (defined as wild-type in both KRAS and NRAS as determined by an FDA-approved test for this use) metastatic colorectal cancer (mCRC):Read More
THE

from a head-to-head phase 3 study, supporting the efficacy of Vectibix® vs Avastin® in WT RAS* left-sided mCRC.
First phase 3 study designed to prospectively compare Vectibix® and Avastin® in combination with mFOLFOX6 for patients with WT RAS* left-sided mCRC1
Head-to-head study (N=823) comparing Vectibix® to Avastin® in combination with chemotherapy in Japanese patients with WT RAS* mCRC and left-sided primary tumors1
First prospective study comparing the effects of biologic therapies in patients with left-sided primary tumors1
Conducting early biomarker testing
to determine a patient’s RAS status
Including tumor sidedness as a criterion
for the selection of biologic therapies
Choosing Vectibix® + FOLFOX
as 1L therapy in newly diagnosed patients
with WT RAS* and left-sided mCRC
*Defined as wild type in both KRAS and NRAS.2
1L = first-line; FOLFOX = fluorouracil, leucovorin, and oxaliplatin; mCRC = metastatic colorectal cancer;
PARADIGM = Panitumumab and RAS, Diagnostically useful Gene Mutation for metastatic colorectal cancer (mCRC); WT = wild type.
Early targeted therapy with Vectibix® + FOLFOX4 improved survival
in newly diagnosed WT RAS* mCRC patients2,3
Median PFS
Months (95% CI)


HR = 0.72 (95% CI: 0.58-0.90)
Median OS
Months (95% CI)


HR = 0.77 (95% CI: 0.64-0.94)
There are no OS or PFS benefits in patients with RAS-mutant mCRC treated with Vectibix®2
PRIME PHASE 3 STUDY DESIGN
PRIME was an open label, randomized (1:1), multicenter study of Vectibix® Q2W + FOLFOX4 vs FOLFOX4 Q2W alone in treatment of newly diagnosed mCRC patients. Among the study population of 1,183 patients with previously untreated mCRC, 656 were WT KRAS† patients. The extended RAS population in the post-hoc analysis consisted of 512 WT RAS* patients. Of these, 259 received Vectibix® + FOLFOX4 and 253 received FOLFOX4 alone.2,3
*Defined as wild type in both KRAS and NRAS.2
†Exon 2 in codons 12 and 13.1
1L = first-line; CI = confidence interval; FOLFOX = fluorouracil, leucovorin, and oxaliplatin; HR = hazard ratio; mCRC = metastatic colorectal cancer; OS = overall survival; PFS = progression-free survival; PRIME = Panitumumab Randomized Trial in Combination With Chemotherapy for Metastatic Colorectal Cancer to Determine Efficacy; Q2W = every 2 weeks; WT = wild type.
Phase 3, randomized, open-label, multicenter study in Japanese patients1
Please see Important Study Considerations below.
Japanese patients with WT RAS† mCRC1
Japanese patients with WT RAS† mCRC1
Primary endpoint1
Secondary endpoints1
Exploratory endpoints1
*Until disease progression, unacceptable toxicity, withdrawal of consent or investigator’s judgement or curative intent resection.1
†Defined as wild type in both KRAS and NRAS.2
‡Adjuvant fluoropyrimidine monotherapy allowed if completed ≥ 24 weeks before enrollment.
§Primary tumor in descending colon, sigmoid colon, rectosigmoid, and rectum.1
DCR = disease control rate; DOR = duration of response; ECOG = Eastern Cooperative Oncology Group; ETS = early tumor shrinkage; FOLFOX = fluorouracil, leucovorin, and oxaliplatin; mCRC = metastatic colorectal cancer; OS = overall survival; PARADIGM = Panitumumab and RAS, Diagnostically useful Gene Mutation for metastatic colorectal cancer (mCRC); PFS = progression-free survival; R0 = curative resection; RR = response rate; WT = wild type.
Vectibix® vs Avastin® in
combination with mFOLFOX6
18% reduction in the risk of death for patients with left-sided tumors treated with Vectibix® vs Avastin®


Vectibix® plus mFOLFOX6 provided a survival benefit vs Avastin® plus mFOLFOX6, reinforcing the clinical value of
Vectibix® as a first-line treatment in patients with WT RAS*, left-sided metastatic colorectal cancer.
*Defined as wild type in both KRAS and NRAS.2
CI = confidence interval; FOLFOX = fluorouracil, leucovorin, and oxaliplatin; HR = hazard ratio; mCRC = metastatic colorectal cancer; WT = wild type.
Vectibix® vs Avastin® in
combination with mFOLFOX6


Analysis was not powered or adjusted for multiplicity to assess efficacy on this endpoint.
Patients who underwent curative resection were censored from the PFS analysis on the final day when
no progressive disease was confirmed. This censoring could have impacted the PFS results.
CI = confidence interval; FOLFOX = fluorouracil, leucovorin, and oxaliplatin; HR = hazard ratio; PFS = progression-free survival.
Vectibix® vs Avastin® in
combination with mFOLFOX6


Analyses were not powered or adjusted for multiplicity to assess efficacy on these endpoints.
*DOR was evaluated in patients with complete or partial response.1
CI = confidence interval; DOR = duration of response; FOLFOX = fluorouracil, leucovorin, and oxaliplatin; R0 = curative resection.
Vectibix® vs Avastin® in
combination with mFOLFOX6


Analysis was not powered or adjusted for multiplicity to assess efficacy in this endpoint.
CI = confidence interval; FOLFOX = fluorouracil, leucovorin, and oxaliplatin.
Vectibix® vs Avastin® in
combination with mFOLFOX6


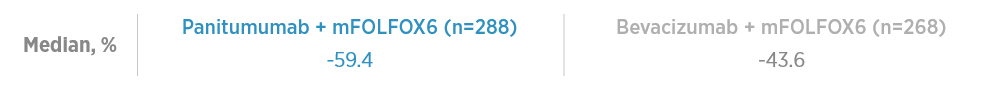
86% of Vectibix®
patients showed a reduction of 30% or more target
lesion size
from baseline.4
Depth of response is defined as the best percentage change from baseline in target lesions. Depth of response evaluated in patients with measurable lesions in baseline.
Horizontal dotted line at ~30% indicates threshold for partial response, a decrease in target lesion size by approximately 30%, as defined by RECIST v1.1.
Predefined exploratory endpoint. Analysis was not powered or adjusted for multiplicity to assess efficacy.
RECIST = Response Evaluation Criteria in Solid Tumors.
Vectibix® vs Avastin® in
combination with mFOLFOX6


Predefined exploratory endpoint. Analysis was not powered or adjusted for multiplicity to assess efficacy.
CI = confidence interval; FOLFOX = fluorouracil, leucovorin, and oxaliplatin; HR = hazard ratio.
Adverse events of any grade ≥ 20% in either treatment arm.1


Dermatological toxicity reactions occurred predominantly in the Vectibix® arm.1 Prophylactic measures may help reduce the severity of dermatologic toxicities.4 Examples of prophylactic skin treatments can be found here.
DOSING

STUDY POPULATION

OUTCOMES
5-FU = fluorouracil; EGFR = epidermal growth factor receptor; mCRC = metastatic colorectal cancer; PARADIGM = Panitumumab and RAS, Diagnostically useful Gene Mutation for metastatic colorectal cancer (mCRC); US = United States; USPI = United States Prescribing Information.


Images are shown for illustrative purposes only
*A hypothetical patient profile of treatment for a newly diagnosed mCRC patient.
ALT = alanine aminotransferase; AST = aspartate aminotransferase; CBC = complete blood count; CT = computed tomography; ECOG PS = Eastern Cooperative Oncology Group Performance Status; Hb = hemoglobin; mCRC = metastatic colorectal cancer; PLT = platelet; WBC: white blood count; WT = wild type.
Medical history
Presentation
Pathology report
Performance status
Laboratory results
Genetic Testing
Imaging results
Surgery consult on metastatic disease
Images are shown for illustrative purposes only
*A hypothetical patient profile of treatment for a newly diagnosed mCRC patient.
ALT = alanine aminotransferase; AST = aspartate aminotransferase; CBC = complete blood count; CT = computed tomography; ECOG PS = Eastern Cooperative Oncology Group Performance Status; Hb = hemoglobin; mCRC = metastatic colorectal cancer; PLT = platelet; WBC: white blood count; WT = wild type.
Dermatologic Toxicity: Dermatologic toxicities occurred in 90% of patients and were severe (NCI-CTC grade 3 and higher) in 15% of patients receiving Vectibix® monotherapy [see Dosage and Administration (2.3), Warnings and Precautions (5.1), and Adverse Reactions (6.1)].
Please see Vectibix® full Prescribing Information, including Boxed WARNING.
Vectibix® is indicated for the treatment of patients with wild-type RAS (defined as wild-type in both KRAS and NRAS as determined by an FDA-approved test for this use) metastatic colorectal cancer (mCRC):
Vectibix® is not indicated for the treatment of patients with RAS-mutant mCRC or for whom RAS mutation status is unknown.
Dermatologic Toxicity: Dermatologic toxicities occurred in 90% of patients and were severe (NCI-CTC grade 3 and higher) in 15% of patients receiving Vectibix® monotherapy [see Dosage and Administration (2.3), Warnings and Precautions (5.1), and Adverse Reactions (6.1)].
References
1. Watanabe J, Muro K, Shitara K, et al. JAMA. 2023;329:1271-1282. 2. Vectibix® (panitumumab) prescribing information, Amgen. 3. Douillard J-Y, Oliner KS, Siena S, et al. N Engl J Med. 2013;369:1023-1034. 4. Yoshino, T. Presented at: 2022 ASCO Annual Meeting; June 3-7, 2022; Chicago, IL. 5. Kobayashi Y, Komatsu Y, Yuki S, et al. Future Oncol. 2015;11:617-627. 6. AVASTIN® (bevacizumab) prescribing information, Genentech. 7. Ma P, Yang BB, Wang YM, et al. J Clin Pharmacol. 2009;49:1142-1156. 8. Chen D, Li L, Zhang X, et al. Medicine (Baltimore). 2018;97:e0097. 9. Arnold D, Lueza B, Douillard JY, et al. Ann Oncol. 2017;28:1713-1729. 10. Tejpar S, Stintzing S, Ciardello F, et al. JAMA Oncol. 2017;3;194-201. 11. Loree JM, Dowers A, Tu D, et al. Clin Cancer Res. 2021;27:52-59.
